Hormonal treatment is considered first line treatment for endometriosis. Although it works for many who have endometriosis symptoms, it also completely misses the mark for other patients.
Why does hormonal treatment not work for everyone with endometriosis? It’s obvious that one size does not fit all, but first, let’s start with the basics.
How does progestin treat endometriosis?
Progestins aim to treat endometriosis by reducing the growth of lesions, in addition to reducing the inflammatory environment created by the lesions3,4.
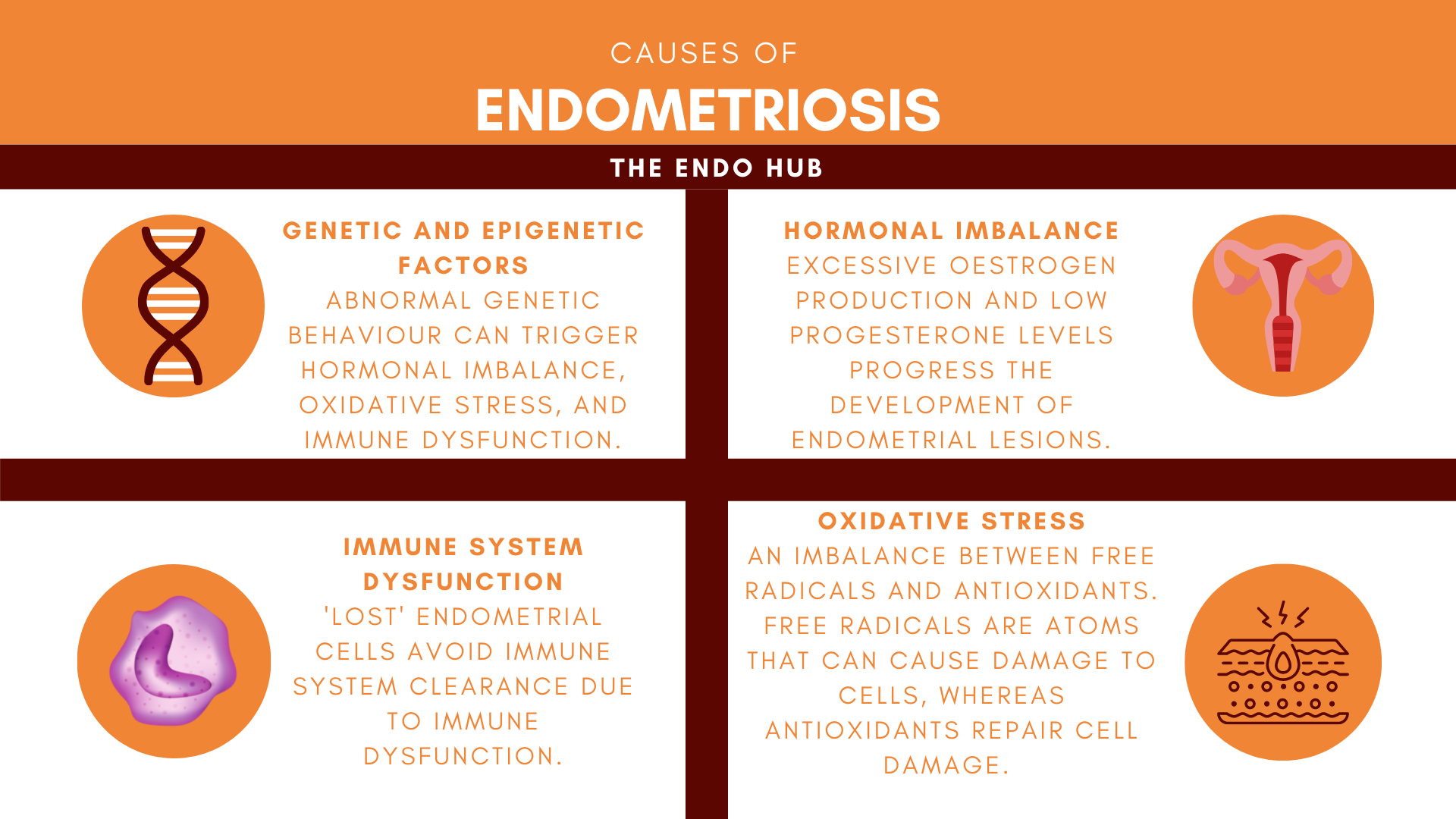
The continuous use of progestins reduces the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which stops menstruation from happening3. Progestins are also thought to stop the release of oestrogens from endometrial lesions, which in turn helps prevent the lesions from increasing in size and also growing more nerves and blood vessels.
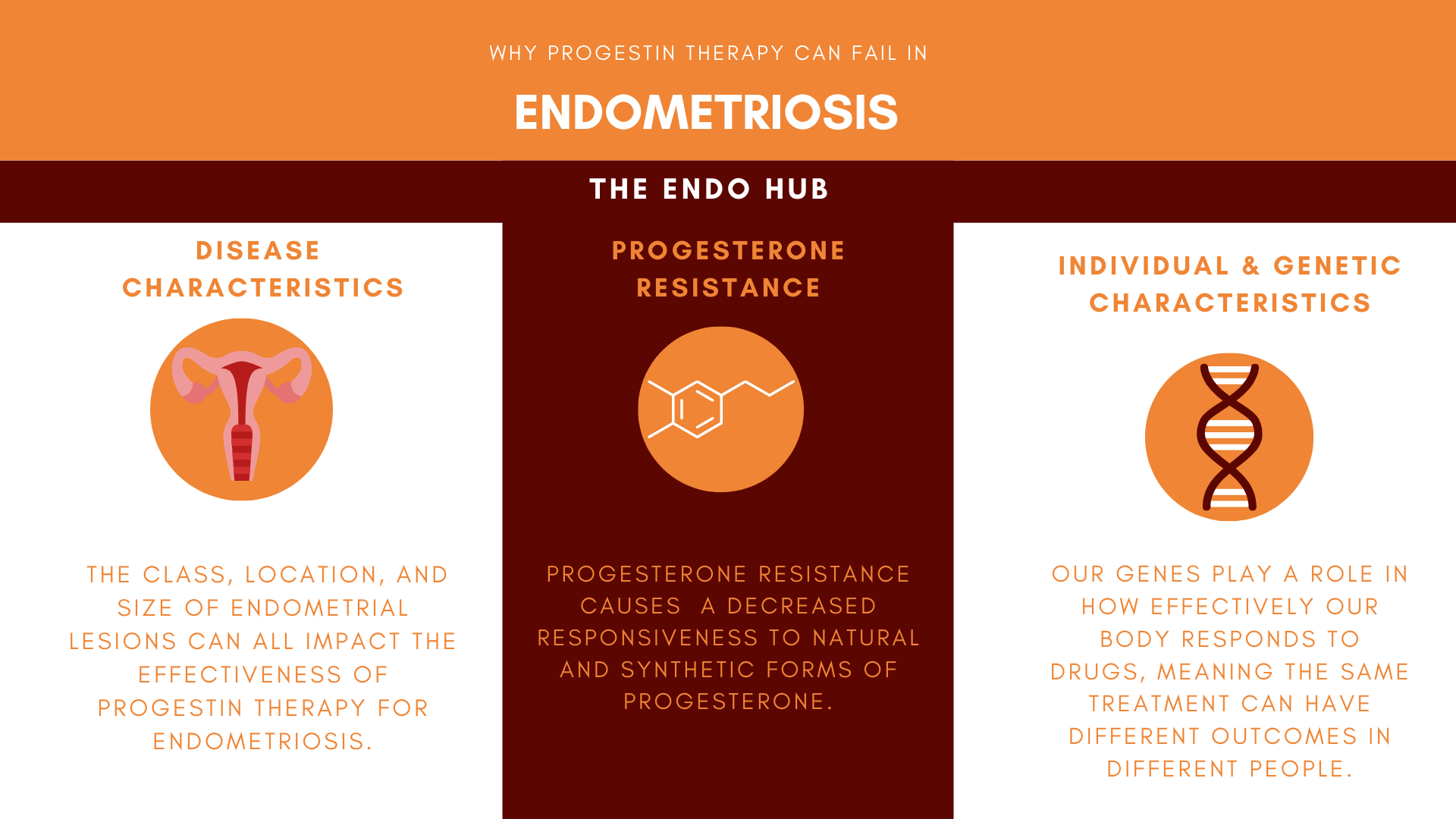
Why can progestin therapy fail?
Disease Characteristics
Not all endometrial lesions are built the same. There are currently 3 different types of endometrial lesions: superficial peritoneal endometriosis (SPE), ovarian endometrioma (OE), and deep infiltrating endometriosis (DIE)5. The different types of lesions are part of what makes endometriosis difficult to treat. Clinical studies for endometriosis often either lump the different types together or focus specifically on one type3. This adds further confusion and makes it unclear whether a type of progestin is effective at treating all types of lesions, equally.
Progestin treatment has been shown to be more effective in reducing blood vessels in superficial lesions than deep infiltrating lesions8. The location of the lesions also changes how well progestin works, too. OE’s have been shown to shrink in size after 6 months of therapy9, whereas DIE lesions have been shown to be more resistant to shrinkage10. Studies have shown that DIE lesions in the intestines have more nerves than DIE found in other locations6, and endometrial lesions in the intestines have been found to continue growing in spite of continuous treatment7.
In summary, the type of endometrial lesion and where it is found can affect how well progestin works and in part explain why progestin therapy does not work for all endometriosis patients3.
Individual characteristics: pharmacogenomics
Pharmacogenomics is the study of how our genes impact how we respond to drugs11. This means we all respond to drugs differently. Our genes play a large role in how well our bodies break down drugs, and how quickly the drugs can be delivered to where they need to go. In order to break down drugs, our bodies use enzymes, and our genes also play a role in how well these enzymes work. This means that in some people, drugs may be broken down poorly, making the drugs not work as well as they should11.
Progesterone Resistance
Progesterone resistance causes progesterone receptors to be less responsive to progesterone and progestins 3,12. Progesterone resistance is a well-known problem in endometriosis treatment and is often thought to be the reason why progestin does not improve symptoms in some patients.
Progesterone Resistance is thought to be caused by genetics or can be brought about by the inflammatory environment that endometrial lesions create 12,13. Certain types of progestins such as Dienogest have been found to be effective against mild progesterone resistance, as it is thought to increase the number of progesterone receptors and decrease inflammation. However, not all progestins are not able to correct the imbalance between oestrogen and progesterone, that progesterone resistance creates13.
Next steps: personalised medicine and innovative treatment
Progestin therapy is thought to treat the symptoms of endometriosis by binding to progesterone receptors to reduce inflammation, the growth of new nerves, and stop further growth of endometrial lesions2. Although progestin therapy works for some patients, it can have short-term relief or no relief in other patients14.
Progestin therapy is often used as a one size fits all treatment for endometriosis, but does not reflect the diversity of the disease. Treatment of endometriosis should take a more personalised approach, which would include finding out the type and location of endometrial lesions, in order to find the best line of treatment possible for every patient.
The genetic profile of patients should also be considered when progestin therapy is being offered, as not all patients will respond to progestin therapy in the same way. All the factors that can impact the effectiveness of progestin therapy should be considered and explained to patients, before it is offered.
References
- NICE, 2021. Hormone treatment for endometriosis symptoms – what are my options?. [online] Nice.org.uk. Available at: https://www.nice.org.uk/guidance/ng73/resources/patient-decision-aid-hormone-treatment-for-endometriosis-symptoms-what-are-my-options-pdf-4595573197
- Gezer, A. and Oral, E., 2015. Progestin Therapy in Endometriosis. Women’s Health, 11(5), pp.643-652.
- Reis, F., Coutinho, L., Vannuccini, S., Batteux, F., Chapron, C. and Petraglia, F., 2020. Progesterone receptor ligands for the treatment of endometriosis: the mechanisms behind therapeutic success and failure. Human Reproduction Update, 26(4), pp.565-585.
- Hill, K., Roemer, S., Churchill, M. and Edwards, D., 2012. Structural and functional analysis of domains of the progesterone receptor. Molecular and Cellular Endocrinology, 348(2), pp.418-429.
- Johnson, N., Hummelshoj, L., Adamson, G., Keckstein, J., Taylor, H., Abrao, M., Bush, D., Kiesel, L., Tamimi, R., Sharpe-Timms, K., Rombauts, L. and Giudice, L., 2016. World Endometriosis Society consensus on the classification of endometriosis. Human Reproduction, 32(2), pp.315-324.
- Wang, G., Tokushige, N., Russell, P., Dubinovsky, S., Markham, R. and Fraser, I., 2009. Hyperinnervation in Intestinal Deep Infiltrating Endometriosis. Journal of Minimally Invasive Gynecology, 16(6), pp.713-719.
- Millochau, J., Abo, C., Darwish, B., Huet, E., Dietrich, G. and Roman, H., 2016. Continuous Amenorrhea May Be Insufficient to Stop the Progression of Colorectal Endometriosis. Journal of Minimally Invasive Gynecology, 23(5), pp.839-842.
- Jondet, M., Vacher-Lavenu, M. and Chapron, C., 2006. Image analysis measurements of the microvascularisation in endometrium, superficial and deep endometriotic tissues. Angiogenesis, 9(4), pp.177-182.
- Taniguchi, F., Enatsu, A., Ikebuchi, A., Yamane, E., Moriyama, M., Murakami, J., Harada, T. and Harada, T., 2017. Efficacy of Norethisterone in Patients with Ovarian Endometrioma. Yonago Acta Medica, 60(3), pp.182-185.
- Leonardo-Pinto, J., Benetti-Pinto, C., Cursino, K. and Yela, D., 2017. Dienogest and deep infiltrating endometriosis: The remission of symptoms is not related to endometriosis nodule remission. European Journal of Obstetrics & Gynecology and Reproductive Biology, 211, pp.108-111.
- Genetics, H. and Research, G., 2021. What is pharmacogenomics?: MedlinePlus Genetics. [online] Medlineplus.gov. Available at: https://medlineplus.gov/genetics/understanding/genomicresearch/pharmacogenomics/
- East-Powell, M., 2021. Low Progesterone and Endometriosis. [online] Endometriosis.net. Available at: https://endometriosis.net/clinical/low-progesterone>
- Green, D., 2021. Progesterone resistance can cause endometriosis. [online] EndoNews.com: News & Research Portal for Endometriosis Foundation of America. Available at: https://www.endonews.com/progesterone-resistance-can-cause-endometriosis
- Bulun, S., Cheng, Y., Yin, P., Imir, G., Utsunomiya, H., Attar, E., Innes, J. and Julie Kim, J., 2006. Progesterone resistance in endometriosis: Link to failure to metabolize estradiol. Molecular and Cellular Endocrinology, 248(1-2), pp.94-103.