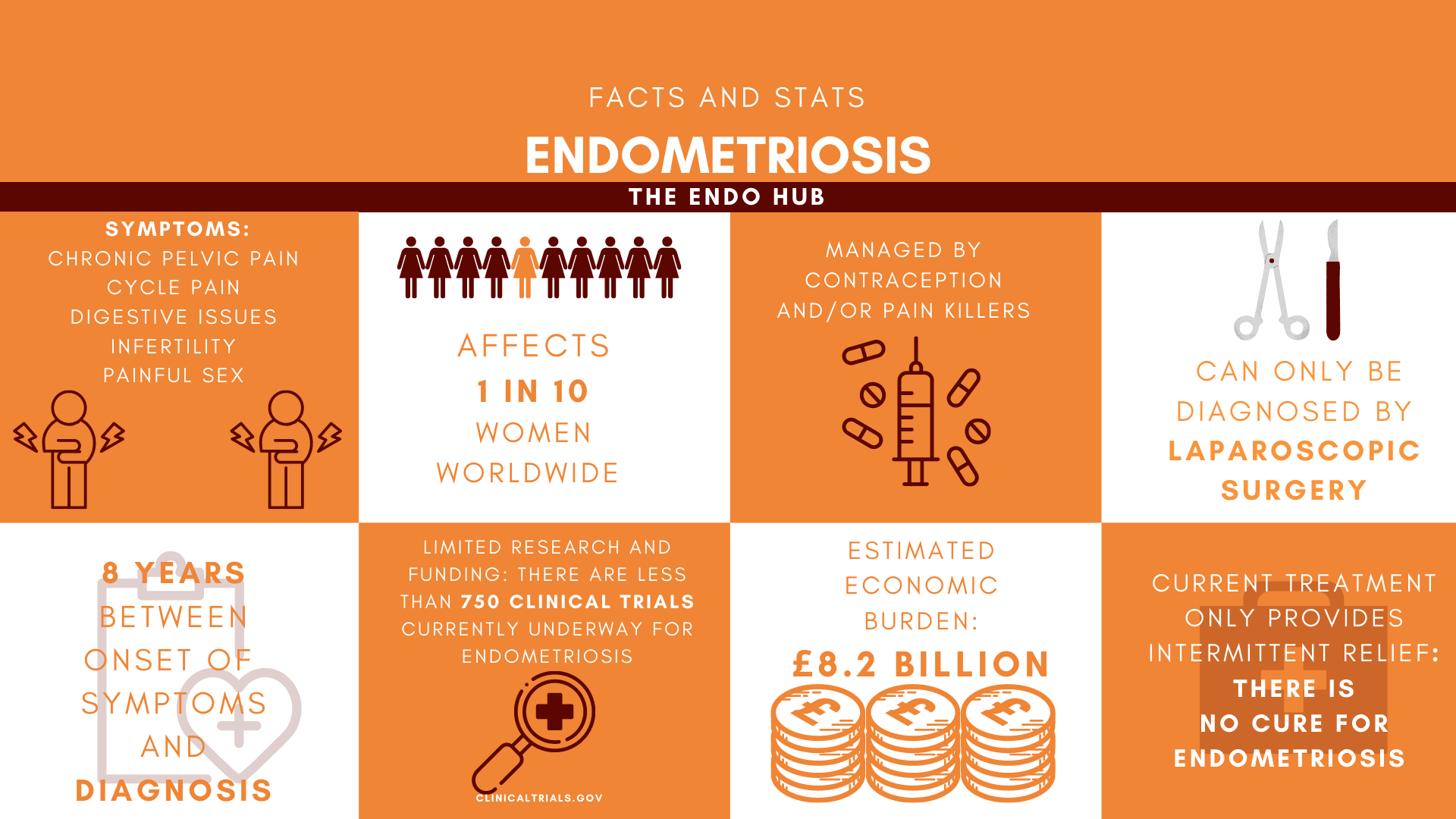
Unless you, or someone you know has it, you probably don’t know what Endometriosis is. Despite the lack of public awareness about the disease, Endometriosis affects 1 in 10 women worldwide.
So, what is Endometriosis?
Endometriosis happens when cells similar to the lining of the uterus (endometrium) are found outside of the uterus, forming patches of tissue (lesions). Lesions can be found on:
- the ovaries
- the peritoneum
- the bladder
- the bowel
- the space between the rectum and vagina (pouch of Douglas)
- the lungs and diaphragm.
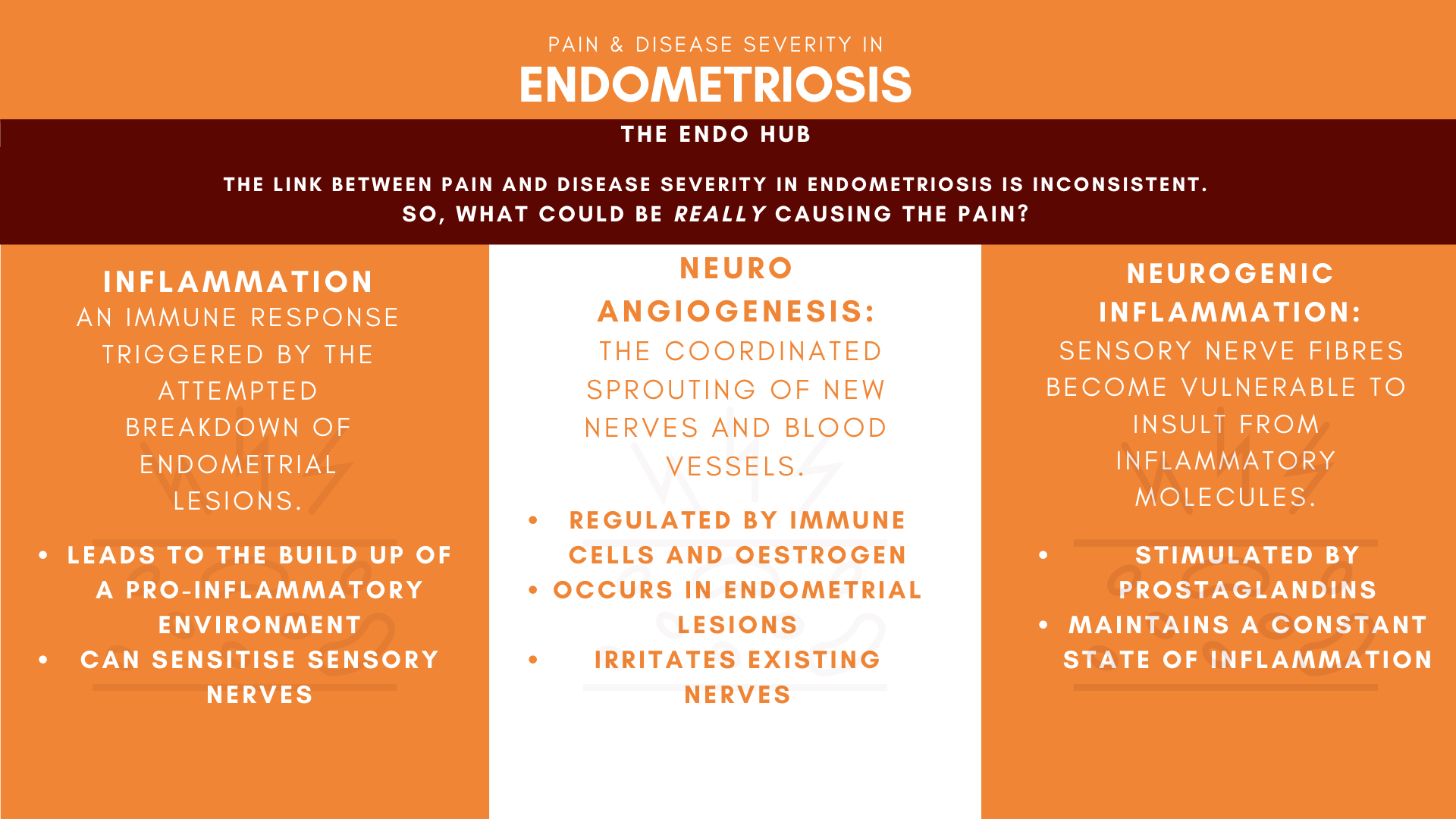
What are the symptoms?
Endometriosis lesions thicken and bleed with every cycle, but the blood has no way to leave the body. This can cause cause symptoms such as:
- Upper abdominal pain
- Pelvic pain
- Painful sex (dyspareunia)
- Painful menstruation (dysmenorrhea)
- Infertility
- Bleeding outside of your period
- Nutrient deficiency
- Painful bowel movements and IBS
- Diarrhoea
- Constipation
- feeling sick (nausea)
- Bloating
- Being sick (vomiting)
- Difficulty/pain while urinating
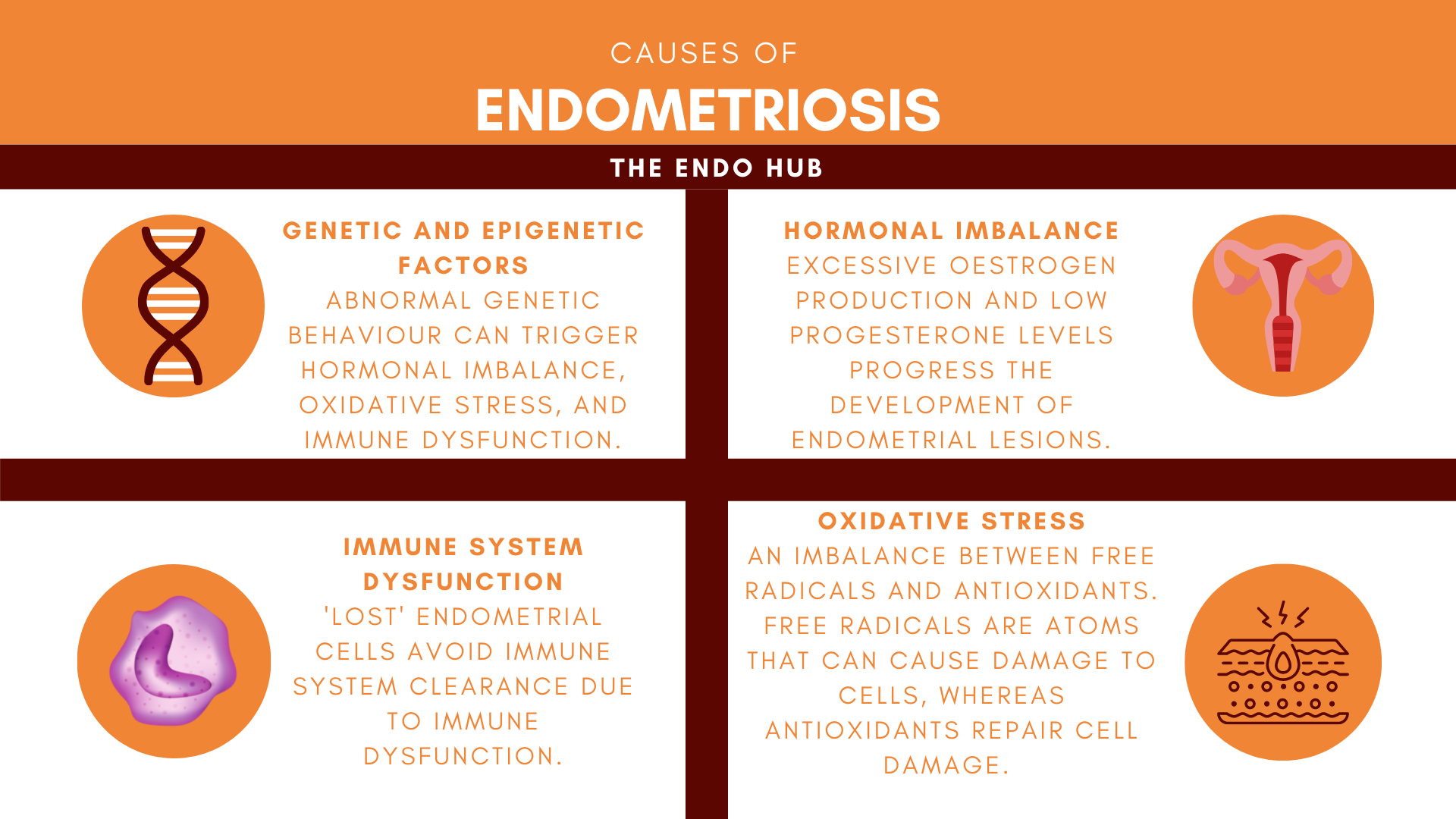
What causes Endometriosis?
The cause of endometriosis is unknown. Retrograde menstruation is the most widely accepted theory.
During your period, the lining of the uterus (endometrium) sheds, causing you to bleed. The retrograde menstruation theory suggests that endometriosis happens due to period blood flowing out of the fallopian tubes and into the pelvis. It is thought that this causes the endometrium to stick to organs in the pelvis.
Although this theory is widely accepted, but, it does not explain:
- why endometriosis does not always worsen with age
- why endometriosis can happen after hysterectomy, or
- the fact that retrograde menstruation occurs in 90% of menstruating women, but endometriosis only occurs in 1 in 10.
Who does it affect?
Endometriosis affects women and people with uteruses of reproductive age (between 12-50). It can also affect post-menopausal women and a small percentage of men, especially those taking oestrogen to treat prostate cancer. The total incidence rate for endometriosis worldwide is estimated to be 176 million, but this does not include those who are yet to be diagnosed.
How is it diagnosed?
Endometriosis can be diagnosed by ultrasound scan, MRI, or keyhole surgery (laparoscopy). It can also be clinically diagnosed based on symptoms only. There is an average wait of 8 years between the onset of symptoms and the final diagnosis for endometriosis in the UK. This could be explained by the normalisation of period pain; the attitudes of health professionals and also the struggle to accurately diagnose endometriosis without laparoscopic surgery.
Although imaging tools such as ultrasound and MRI can be of help, most imaging tools are not strong enough to detect smaller endometrial lesions. A study conducted in South-East England found only 10.6% of their patients to be accurately diagnosed with Endometriosis via ultrasound.
What are the treatment options?
There is no cure for endometriosis. There are only three treatment options available: hormonal, non-hormonal, and surgical. These treatments aim to reduce the symptoms of endometriosis.
Hormonal treatment: using hormones to stop you from having periods and slow the growth of endometriosis. Side effects of this treatment include:
- low mood (depression)
- anxiety
- decreased bone density
- increased risk of breast cancer
Non-hormonal treatment: using painkillers to reduce pain and inflammation caused by endometriosis. The side effects vary depending on the side effects of the pain killers used, which can include:
- constipation
- drowsiness
- stomach ulcers
- your body getting used to the painkillers (tolerance)
Surgical treatment: This can include:
- cutting out endometrial lesions (excision)
- burning the lesions (ablation) or
- removal of the uterus (hysterectomy).
Surgery may lead to further complications depending on the locations of the lesions, as well as the experience level of the surgeon.
Can pregnancy cure endometriosis?
Some healthcare professionals may suggest pregnancy as a solution to endometriosis, however, this only may provide temporary relief, which is not guaranteed.
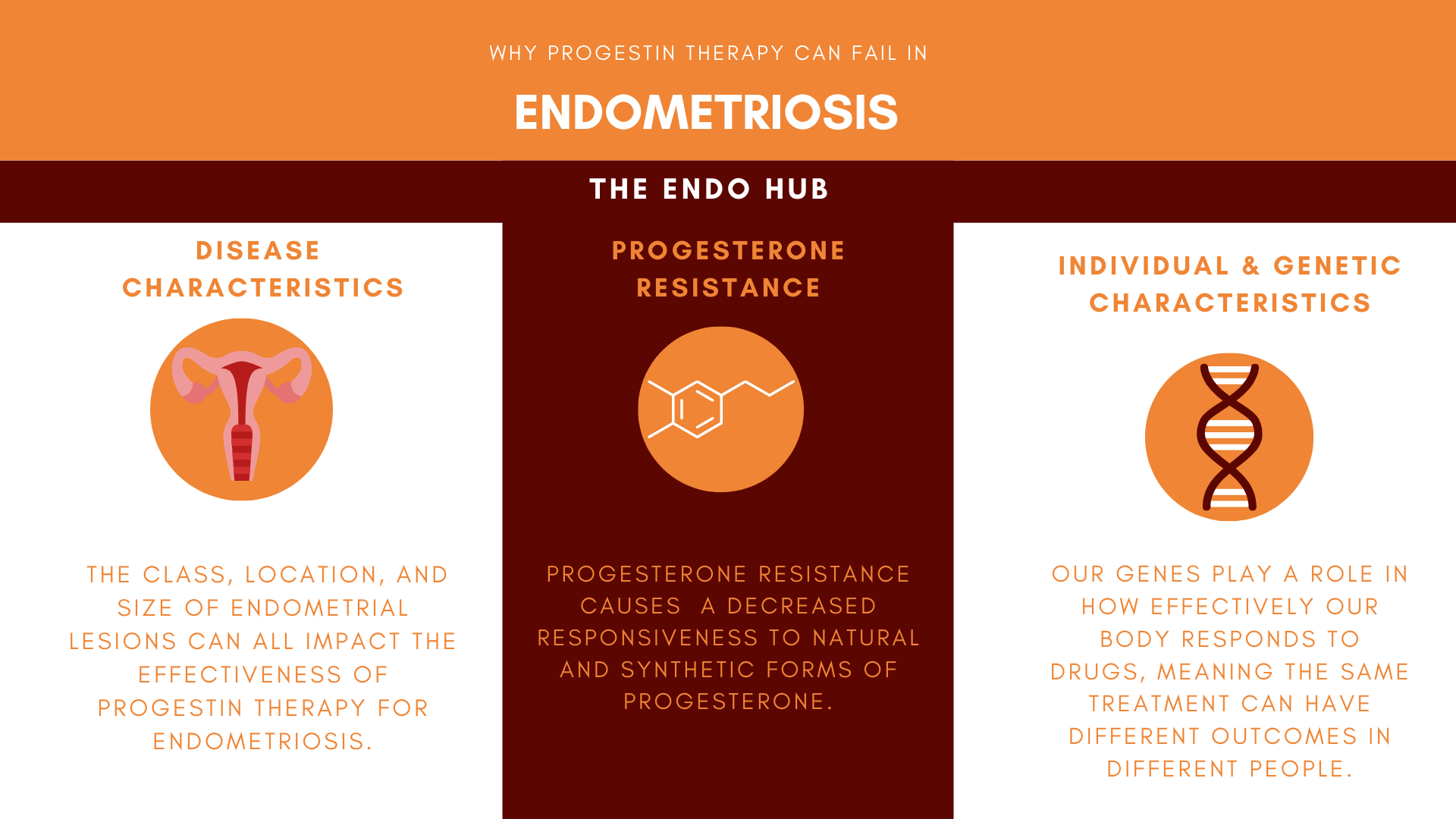
There is no ‘One-Size-Fits-All’ when it comes to treatment for endometriosis. Some treatments work for some patients and not for others.
The Bottom Line
Living with endometriosis can have a large effect on your mental, physical, and social well-being.
The attitudes of healthcare professionals towards women’s health and the normalisation of period pain also have a large role to play in the poor diagnosis and treatment of endometriosis.
Despite 176 million (and counting) living with this disease worldwide, the reason endometriosis happens is still unknown. This limits the treatment options for the disease. More research into individualised care for endometriosis needs to be done to change this.
Stay tuned for more articles about endometriosis!
Super informative, can’t wait for more articles!
Thank you for providing such a detailed and informative yet simple explanation on endometriosis ! Will be sharing to spread awareness